View Dr. Joe Gerald’s Weekly Epidemiology & Hospital Occupancy Report
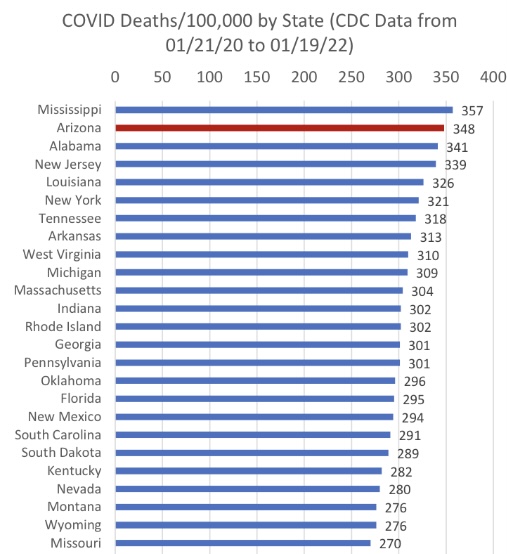
Arizona blew through the 26,000 COVID death mark this week. Weekly death totals in the upper-300s, mid-400s are likely for several more weeks. Arizona still stands in 2nd place in COVID deaths per capita, trailing only Mississippi.
Within 2-3 weeks Arizona will have the distinction of being:
#1 in COVID deaths per capita (once we pass Mississippi)
#1 in increased all-cause mortality over baseline
The only state in which COVID19 is the leading cause of death
COVID-19 hospital occupancy continues its march upward in the face of no mitigation policy from Governor Ducey & Interim Director Herrington. Hospitals are burdened by >30% occupancy in general wards and in the ICU. Access to care continues to be restricted by both COVID-19 occupancy and staff shortages because of infections among healthcare workers (or their family members).
Arizona continues to have historic levels of community transmission attributable to Omicron and the lack of mitigation policies. Test positivity is incredibly high reminding us that test capacity, accessibility, and/or uptake is wholly inadequate.
As of January 23rd, new cases were being diagnosed at a rate of 1694 cases per 100K residents per week. Rates peaked last week at ~1967 cases per 100K/week, somewhat lower than some other states, perhaps due to less testing. The risk of Omicron infection will remain extremely high for many weeks. Remember, the CDC defines high community transmission as levels >100 cases per 100K residents per week. We’re a far cry from that!
View Dr. Joe Gerald’s Weekly Epidemiology & Hospital Occupancy Report