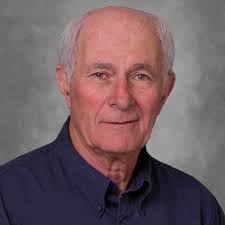
In an informative & entertaining interview with KJZZ, AZPHA member, former AHCCCS director and longtime public health advocate Dr. Len Kirschner offered an AHCCCS history lesson and a frank warning about the real-life consequences of proposed Medicaid cuts in Arizona.
‘It’s gonna have a terrible outcome’: What this former AHCCCS director says about Medicaid cuts
In the spot, Kirschner uses his decades of experience to explain how the coming Medicaid budget cuts will unravel critical safety nets for Arizona’s most vulnerable residents.
Dr. Kirschner outlines the financial and human costs of scaling back Medicaid and reminds us what’s at stake for public health, preventive care, and long-term community well-being.
See also: House Budget Resolution Threatens Big Medicaid (AHCCCS) Cuts – AZ Public Health Association & New Fiscal Analysis: The Economic Impact of Federal Medicaid Cuts in Arizona – AZ Public Health Association