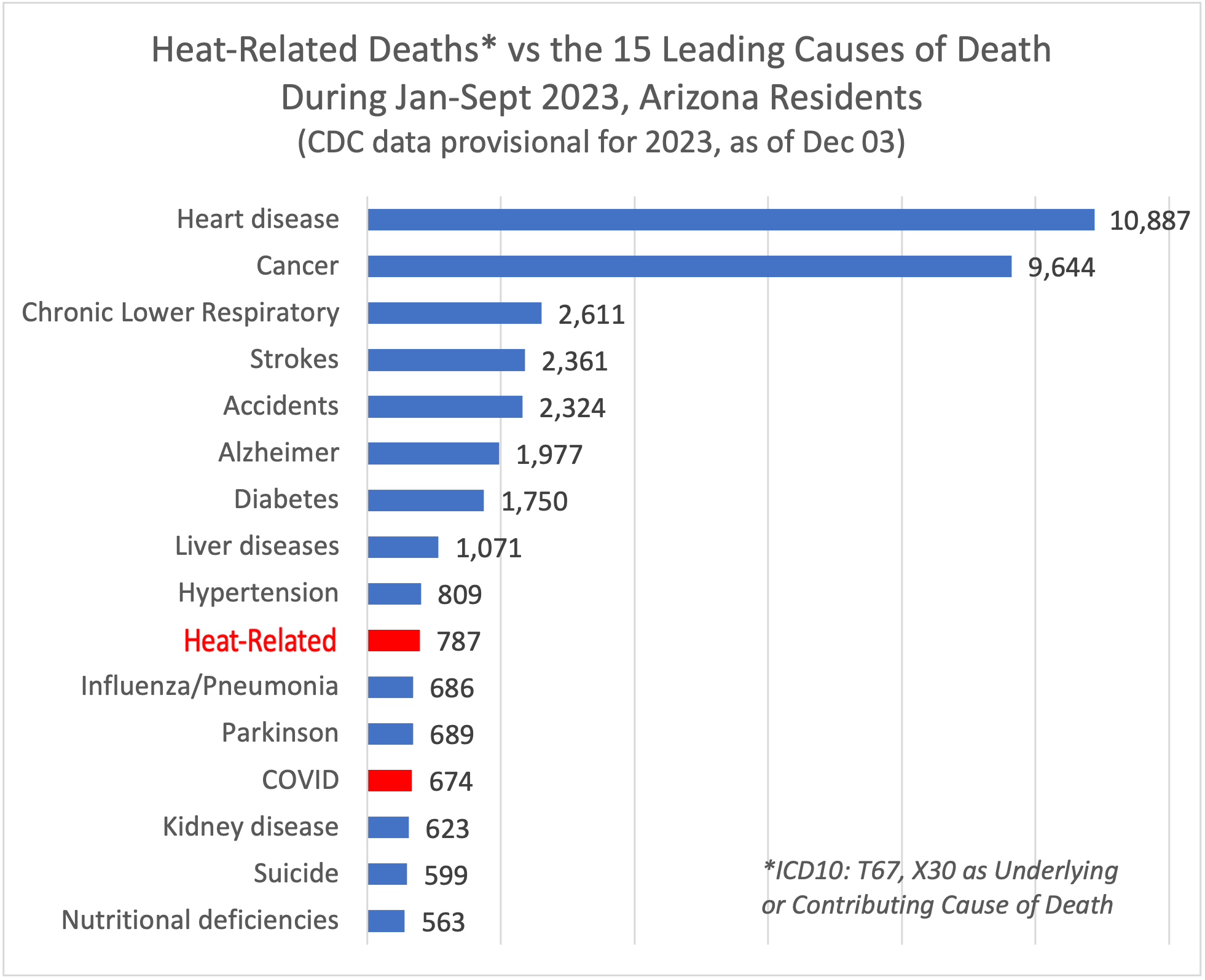
1. Heart Disease (10,887)
- Don’t smoke
- Exercise regularly
- Manage blood pressure
- Manage cholesterol levels
- Lower salt/alcohol use
- Better nutrition
2. Cancer (9,644)
- Don’t smoke
- Eat well balanced diet
- Physical activity
- Get routine screenings
- Use sunscreen/protect skin
- Get regular checkups
3. Chronic Lower Respiratory Illnesses (2,611)
- Don’t smoke
- Worker safety protection
- Keep up to date with vaccines
- Exercise
4. Stroke (2,362)
- Don’t smoke
- Manage blood pressure
- Lower alcohol use
- Better nutrition
- Seek treatment medication for AFIB (atrial fibrillation)
- Regular checkups
5. Accidents (2,324)
- Buckle up
- Drive a safe car with airbags
- Don’t drive under the influence
- Avoid recreational use of pills (fentanyl)
- In home fall prevention strategies
- Physical activity/balance
6. Alzheimer’s (1,977)
7. Diabetes (1,750)
- Manage the disease
- Physical activity/nutrition
- Don’t smoke
- Manage blood pressure/cholesterol
- Modest alcohol use
8. Liver Disease (1,071)
- Getting vaccinated for Hepatitis A and B
- Practicing good hygiene
- Drinking alcohol in moderation
- Use medications as directed
- Get routine checkups with blood tests
- Practice harm reduction if you’ve had Hep C
9. Hypertension (809)
- Get regular checkups & take medicine as directed
- Don’t smoke
- Lower salt intake
- Improve physical activity & nutrition
- Limit alcohol
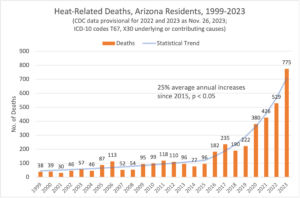
10. Heat (775)
- Strategies to reduce homelessness
- Increase affordable housing
- Limit outdoor exposure to extreme heat
- Stay hydrated
11. Influenza/Pneumonia (686)
- Stay up to date on all vaccines including influenza, COVID-19, pneumonia etc.
- Get routine checkups
12. Parkinsons (689)
13. COVID-19 (674)
- Get most up to date booster vaccines for COVID-19
14. Kidney Disease (623)
- Stay active
- Manage diabetes
- Take medication as directed
- Eat a healthy diet
- Reduce salt intake
- Don’t smoke
- Check and control your blood sugar and blood pressure as part of your regular checkups
- Get your kidney function checked if you have one or more of the ‘high risk’ factors: diabetes, hypertension, obesity, a family history.
15. Suicide (599)
- Depression screening
- Seek behavioral health help
- Improve social connectedness
- Identify persons at risk
- Evidence based responses
- Enhance life skills and resilience
16. Nutritional Deficiency (seniors – usually protein deficiency) 563
- Eat healthy diet with enough protein
- Manage diet as you age
- Sufficient nutrition