New Tribal Area Health Education Center in the Works
Last session the state legislature passed a bill authorizing a sixth Arizona Regional Center Area Health Education Center (AHEC) that will focus on the American Indian health system and workforce. Its creation was the culmination of the hard work of many organizations and individuals, none more so than Kim Russell, Human Services Coordinator at the Inter-tribal Council of Arizona.
In concert with the other five regional AHECs, the Arizona American Indian AHEC will support the overall mission to enhance access to quality health care, particularly primary and preventive care, by improving the supply and distribution of health care professionals through academic/community educational partnerships in rural and urban medically underserved areas.
The Arizona AHECs major funded activities include:
- Youth (Grades K-16 Health Career Pipeline Programs) introduces Arizona’s youth to health careers
- Health Professions Trainee Education includes clinical rotations, also called field experiences
- AHEC Scholars Community Interprofessional Community Immersion
- Continuing Education for working health professionals
- Community Health Promotion for health education activities and events for community members
Tribal partners are currently meeting to prepare a request for proposal for the creation of the new Tribal AHEC Regional Center in early 2022. To learn more about the Arizona American Indian AHEC, please visit: https://azahec.uahs.
Now that Arizona Is In Crisis Standards of Care (for the Most Critically Ill COVID Patients), How Will Doctors Allocate Treatment?
Now that each and every extracorporeal membrane oxygenation (ECMO) machine in Arizona is being used, we are essentially in Crisis Standards of Care, at least for the most critically ill COVID patients (ECMO machines are the last resort for COVID patients in severe respiratory failure).
“Crisis Standards of Care” is basically a protocol for making healthcare decisions when the system can’t provide all of the care that everybody needs because the needs outstrip the resources. It’s a protocol to help healthcare providers objectively decide who gets care when resources don’t allow everyone to get treatment.
Arizona has two documents that outline how doctors are supposed to make life and death decisions because there aren’t enough resources to treat all patients.
Arizona Crisis Standards of Care – Full Document
Arizona Crisis Standards of Care Addendum April 2021
The reports specify statewide triage protocols to use when demand outstrips supply. It has a section on “Stabilization of Patients Awaiting Triage” and “Triage Protocols for Scarce Resource Allocation”. From a big picture point of view, all patients who can potentially benefit from therapies are offered treatment when resources are sufficient, but when resources aren’t (as is the case right now for patients in respiratory failure), patients get assessed to determine how best to allocate care. The documents outline objective triage protocols to make those decisions (called tertiary triage).
The Crisis Standards of Care protocol uses a stepwise scoring system process to determine how to prioritize patients. People with lower scores would be a higher priority for treatment because they’re more likely to survive.
Patients with lower scores would be given priority for care (see the reports for details). But sometimes, several people might have the same score (color coding). If that happens, the protocol says that additional factors may be considered as priorities. Those priorities include:
-
Pediatric patients < 18 years of age;
-
First responders or front-line healthcare workers;
-
Single caretakers for minors or dependent adults;
-
Pregnant patients; and
-
Short-term survival to hospital discharge based on clinical judgement, provided this judgement is made
without regard to basis of race, ethnicity, color, national origin, religion, sex, disability, veteran status,
age, genetic information, sexual orientation, gender identity, perceived quality of life, resource intensity/duration, perceived social worth, or any other ethically irrelevant criteria.
This is our new reality folks, again. Sadly, it didn’t have to be this way if only Governor Ducey had used evidence-based policies to incentivize vaccination (e.g. vaccination mandates) and other tools like universal masking requirements in public indoor environments.
President Outlines Updated Federal COVID Interventions
Last week the President outlined a number of new interventions designed to mitigate COVID spread this winter. Here’s an outline of what was announced last week. The intervention plan includes the following categories:
- Boosters for All Adults
- Vaccinations to Protect Our Kids and Keep Our Schools Open
- Expanding Free At-Home Testing for Americans
- Stronger Public Health Protocols for Safe International Travel
- Protections in Workplaces to Keep Our Economy Open
- Rapid Response Teams to Help Battle Rising Cases
- Supplying Treatment Pills to Help Prevent Hospitalizations and Death
- Continued Commitment to Global Vaccination Efforts
- Steps to Ensure We Are Prepared for All Scenarios
I won’t go into the particulars here (you can review for yourself) but among the most significant are that private health insurance plans will be required to reimburse for buying home test kits. Test kits will be free at community health centers, and there will be more outreach/access points of adult boosters and childhood vaccines.
The requirement that in-bound jet passengers test negative 24 hours before departure (regardless of vaccination status) makes sense but the complete ban on inbound travel from 8 African countries makes no sense, particularly in light of the requirement for a negative test 24 hours before departure.
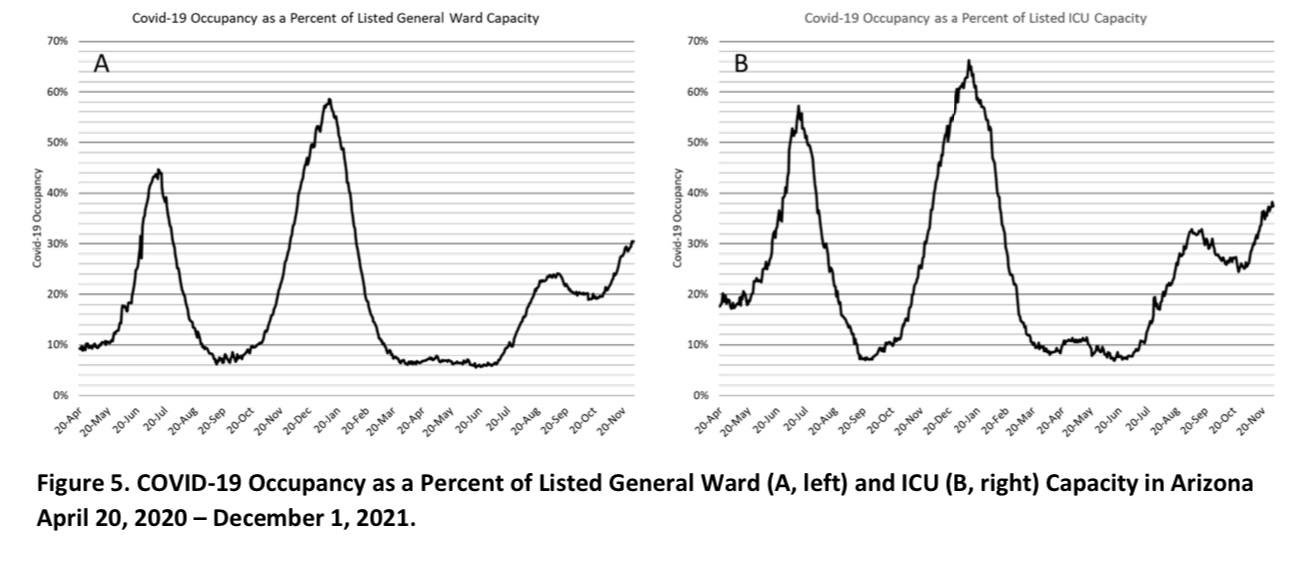
Arizona Hospitals Under Contingency Standards of Care as Nearly 40% of Arizona ICU Beds Are Now COVID Patients
View Dr. Joe Gerald’s Weekly COVID Epidemiology & Hospital Occupancy Analysis
How Big of a Deal is the Omicron Variant?
There’s been no shortage of doomsayers when it comes the discovery of the Omicron. The truth is that we don’t know enough yet to assess what the public health impact of Omicron will be compared with Delta. Yet.
The keys to making that determination depend on:
- How transmissible Omicron is;
- What the clinical presentation is for persons with an Omicron infection (compared to Delta); and
- Whether immunity people have built from vaccinations or previous infections provide substantial protection from being infected with or having a bad outcome from Omicron.
The main way that Omicron could displace Delta is if it’s more transmissible than Delta (currently 99% of global infections are Delta). If Omicron is less transmissible (regardless of the clinical symptoms Omicron presents) then Omicron will likely die out. If Omicron is slightly less transmissible than Delta, but substantially evades immunity people have previously acquired, then Omicron might be able to compete with Delta. If Omicron is more transmissible than Delta (regardless of clinical presentation and immunity escape) it will take over (like Delta displaced Alpha).
Another key piece of information we’ve yet to discover is just how dangerous Omicron is compared with Delta. Is an Omicron infection worse than outcome that Delta (and if so- in what populations)?
Is Omicron Worse than Delta? There Are 3 Possibilities
Omicron could be less dangerous to public health than Delta if it’s more transmissible, has a milder clinical presentation, and if previously acquired immunity still provides protection from infection and bad clinical outcomes.
Omicron could be a wash if it’s less transmissible than Delta and previously acquired immunity still provides protection. In that case, Omicron will die out too. Omicron could end up being about as transmissible as Delta, have a similar clinical presentation to Delta, and be substantially covered by acquired immunity – in which case Delta and Omicron could replicate side by side without a substantial change in public health impact.
Omicron could be more dangerous if it’s more transmissible and has the same or worse clinical presentation compared to Delta and/or escapes previously acquired immunity. If Omicron has a substantially worse clinical presentation and is more transmissible than Delta- that would be really bad.
The point is that we don’t have enough information from the ongoing epidemiological investigation in the Republic of South Africa to determine whether Omicron poses the same, more, or less threat compared to Delta. The Republic of South Africa has impressive research institutions and a competent national health department- so before December is over, we should have the answers to those 3 key aspects:
- Transmissibility;
- Clinical Presentation; and
- Immunity escape.
Those pieces of information will tell us whether Omicron is a bad thing, a good thing, or a wash.
Build Back Better Act Is a Boon For A Transition to Clean Energy
If signed into law, the Build Back Better Act would set the United States on a path to a 50-52% reduction in carbon pollution by 2030. That’s the same goal scientists say is necessary to prevent the worst impacts of climate change.
Here what’s included in this historic legislation that will put the U.S. on the path to cutting our climate pollution in half by 2030, invest directly in communities of color too often left behind, and create good-paying jobs.
- Electric Vehicles: Includes tax credits for consumers who purchase EVs of up to $12,500 per vehicle. These incentives would have a critical impact on climate and air pollution by inducing rapid market transformation, and improve air quality in high traffic areas.
- Electric Vehicle Charging: Builds a 500,000 electric vehicle charging stations in communities nationwide. Along with a clean grid, rapid electrification of passenger vehicles and medium- and heavy-duty trucks would prevent 150,000 pollution-related deaths and save consumers $2.7 trillion by 2050.
- Home Energy Efficiency: Enables working & middle-class families to save up to $8,000 while weatherizing their homes to reduce utility bills and pollution.
- Lower Energy Bills: Helps the average family save about $500 each year in utility bills.
- Clean Air: Converts more than 60,000 diesel school buses to clean electric buses so schoolchildren can breathe clean air, and convert 70% of U.S.P.S. mail trucks to electric vehicles to reduce air and climate pollution in your neighborhood
- Clean Water: Helps replace over 5 million lead service lines to deliver clean water to neighborhoods nationwide
- Job Training: BBB Act training programs will prepare Arizona’s workers for high-quality jobs in fast-growing sectors like public health, childcare, manufacturing, IT, and clean energy. Nineteen Arizona community colleges will have the opportunity to benefit from grants to develop and deliver innovative training programs and expand proven ones.
2022 National Health Service Corps Loan Repayment Programs Accepting Applications
The Health Resources & Services Administration’s National Health Service Corps (NHSC) is accepting applications for its loan repayment programs for its fall cycle. There has been a substantial increase in funding available this year… so there are more opportunities than ever in this important public health workforce program!
- NHSC Loan Repayment Program – awards up to $50,000 in exchange for a two-year commitment to provide primary medical, dental or mental/behavioral healthcare at approved sites in high-need, underserved areas.
- NHSC Substance Use Disorder (SUD) Workforce Loan Repayment Program – provides up to $75,000 in exchange for a three-year commitment to healthcare professionals who provide substance use disorder treatment services.
- NHSC Rural Community Loan Repayment Program – awards up to $100,000 for three years of service to providers in rural communities.
To apply, click here.
Public Health Workforce Federal Loan Forgiveness Program
Last week the U.S Department of Education announced a program that provides temporary relief to current and future Public Service Loan Forgiveness program participants as a result of the COVID-19 pandemic.
Public health workers that borrowed money for school under the PSLF program can get credit for past ‘non-qualifying payments’. Under the new rules, “any prior payment made will count as a qualifying payment, regardless of loan type, repayment plan, or whether the payment was made in full or on time”. The change applies to student loan borrowers with Direct Loans, those who have already consolidated into the Direct Loan Program, and those who will consolidate into the Direct Loan Program.
The Department of Education will credit borrowers for prior payments made while working for a qualifying employer like a county or state health department regardless of loan type or repayment plan. To participate, borrowers need to submit this form by Oct. 31, 2022.
Temporary Loan Forgiveness Highlights
- What are the new rules?
- Do I qualify for additional payments?
- What next steps should I take?
- What if I have other questions?
- Use the PSLF Help Tool.
What Are the Return on Investments for the Meds that Treat & Prevent COVID-19?
With two potential new medications to treat COVID19 infections on the horizon, I thought I’d do an estimate of the financial return on investment for the various treatments and compare that to the ROI for the vaccines. Here goes:
Average COVID19 Hospitalization Costs
To do the back of the envelope ROI math, we’ll need to start with what an average COVID-19 hospitalization costs for unvaccinated persons. CMS found that the Average Medicare payment per fee-for-service COVID-19 hospitalized Medicare beneficiary is $24,033 (see this COVID19 Data Snapshot Public Release). According to Fair Health, an independent nonprofit focused on enhancing price transparency in healthcare, the average charge for COVID-19 hospitalization in Arizona is $361K for complex patients and $42K for non-complex patients. To be conservative, let’s go with the number from CMS… $24K.
Return on Investment for Regeneron
Let’s start with Regeneron, the monoclonal antibody treatment for which governor Ducey is such an enthusiast. Regeneron’s clinical trial found that their hospital-administered monoclonal antibody treatment reduces COVID-19-related hospitalization or deaths in high-risk patients by about 70%.
The federal government pays Regeneron Pharmaceuticals $2,100 per treatment course for the drug. Because it needs to be administered in a clinical setting, the actual full cost of a treatment course is about $10,000.
If Regeneron were administered to 1,000 patients at high risk of a bad outcome and it’s truly 70% effective at preventing hospitalization, Regeneron would bring down hospital costs from $24M to about $7.2M, a hospitalization savings of about $16.8M. Regeneron costs about $10M to administer to 1,000 patients… so we need to add that in to the costs too. At 70% effectiveness, the ROI for Regeneron would be about 1.6. In other words, for every dollar we spend on Regeneron administration to patients at high risk of hospitalization we only get $1.60 back in reduced hospital costs for COVID patients.
Editorial Note: Regeneron is being over-administered in Arizona. Low-risk persons are routinely receiving treatment with Regeneron because of the financial incentives established by Governor Ducey in this Executive Order. The ADHS is reinforcing the over-administration of Regeneron by peppering their letters to hospitals (which they regulate) encouraging Regeneron administration. Because this very expensive treatment is routinely being administered to low-risk persons, the ROI for Regeneron is actually below 1.
Return on Investment for the New Antivirals
Both Merck and Pfizer have stated that they have developed antiviral pills that are about 90% effective at preventing hospitalization from a COVID-19 infection if taken early in the infection. Both companies have asked the FDA for emergency use authorization of their new medications, but neither have published their trial data in a peer-reviewed journal.
The FDA is holding a meeting of their Antimicrobial Drugs Advisory Committee Meeting today to discuss Merck’s antiviral (molnupiravir) pills for treatment of COVID-19. View the evidence published by the FDA on this application here.
The use of Merck & Pfizer antivirals haven’t been authorized yet, but the federal government has already contracted with Pfizer $529 and Merck $700 per treatment course.
Let’s assume that the materials the FDA just posted are correct, and Merck’s pills are 90% effective at preventing hospitalization or death among patients that are high-risk for hospitalization. If either of these medications were administered to 1,000 patients that would have otherwise been hospitalized (and the meds are really 90% effective) the drugs would bring down hospital costs from $24M to about $2.4M, a savings of about $21.6M.
But… the drugs will cost an average of $600 to administer to each person ($600,000 total for 1,000 people), so at 90% effectiveness and $600 per treatment regimen, the ROI for these antivirals would be about 40 if given only to patients at high-risk for hospitalization. In other words, for every dollar we spend on the future Merck or Pfizer antiviral pills we’d get about $40 back in reduced hospital costs among high-risk COVID patients.
Return on Investment for Vaccines
The federal government’s contract with Pfizer, Moderna, and Johnson & Johnson is about $20 per vaccine dose. There’s also an administration cost for the vaccine. For example, Medicare reimburses providers $40 per COVID19 vaccine administered.
Putting those costs together, a 2-dose series of the mRNA vaccine costs the taxpayers about $120. The mRNA vaccines are more than 95% effective at preventing hospitalization, but to be conservative, let’s say it’s just 90%.
When either of the mRNA vaccines are administered to 1,000 people who would have otherwise become infected and hospitalized (even at only at 90% effectiveness), hospital costs would go down from $24M to about $2.4M, a savings of $21.6M.
The vaccines cost an average of $120 to administer to each person ($120,000 total for 1,000 people), so at 90% effectiveness and $120 per full vaccination the ROI for the mRNA vaccines would be about 180. In other words, for every dollar we spend on vaccinating folks with the mRNA vaccines we’d get $180 back in reduced hospital costs for COVID patients. (Note: the ROI is actually higher than 180 because vaccines not only prevent bad outcomes but also reduce community spread).
Editorial Note: Vaccines are far and away the most cost-effective way to save lives and reduce healthcare costs. The President is doing what he can to implement policies that will drive up vaccination rates via the new OSHA and CMS regulations. Governor Ducey and Attorney General Brnovich, on the other hand, are doing what they can to stop the White House proposals and are actively taking steps to prevent vaccination requirements.
A true fiscal conservative would look at the 180+ ROI for vaccines, compare that to the 1.6 ROI for Regeneron and do everything he or she could to get more people vaccinated.